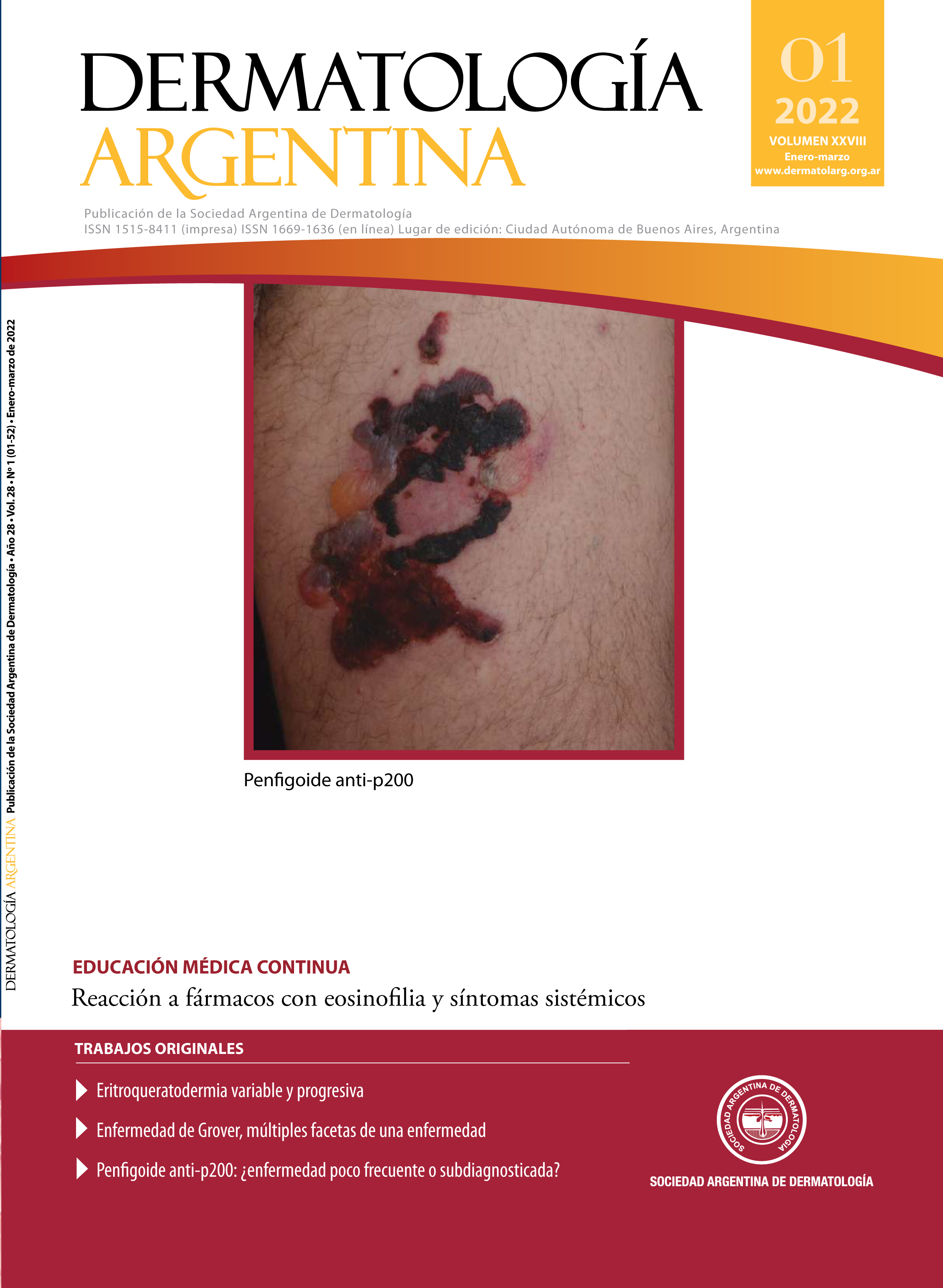
Drug reaction with eosinophilia and systemic symptoms (DRESS)
DOI:
https://doi.org/10.47196/da.v28i1.2246Keywords:
DRESS, adverse drug reaction, eosinophiliaAbstract
Drug reaction with eosinophilia and systemic symptoms (DRESS) or drug-induced hypersensitivity syndrome (DIHS), is a serious and rare adverse drug reaction. Among the mechanisms involved in its pathophysiology, there are various alterations in drug-metabolizing enzymes with the consequent accumulation of reactive metabolites, sequential reactivation of viruses of the herpes family, genetic predisposition associated with certain HLA, and a type IV hypersensitivity response. Currently, new drugs responsible for this pathology have been incorporated, such as biologicals, immunosuppressants and chemotherapy. The clinical presentation of DRESS is variable. It has a high morbidity and mortality and involves high costs in medical care. Its treatment consists, in the first place, in the suspension of the causal or suspected drugs. Then, depending on severity, systemic corticosteroids or IVIG combined with corticosteroids, plasmapheresis, cyclosporine, mycophenolate mofetil, and rituximab may be indicated.
The objective of this work was review DRESS and highlight the new and relevant aspects of the last 5 years.
References
I. Shiohara T, Mizukawa Y. Drug-induced hypersensitivity syndrome (DiHS)/drug reaction with eosinophilia and systemic symptoms (DRESS): An update in 2019. Allergol Int. 2019;68:301-308.
II. Watanabe H. Recent advances in drug-induced hypersensitivity syndrome/drug reaction with eosinophilia and systemic symptoms. J Immunol Res. 2018;2018:5163129.
III. Kardaun SH, Sekula P, Valeyrie-Allanore L, Liss Y, et ál. Drug reaction with eosinophilia and systemic symptoms (DRESS): an original multisystem adverse drug reaction. Results from the prospective RegiSCAR study. Br J Dermatol. 2013;169:1071-1080.
IV. Mushiroda T, Takahashi Y, Onuma T, Yamamoto Y, et ál. Association of HLA-A*31:01 Screening With the Incidence of Carbamazepine-Induced Cutaneous Adverse Reactions in a Japanese Population. JAMA Neurol. 2018;75:842-849.
V. Alfirevic A, Pirmohamed M, Marinovic B, Harcourt-Smith L, et ál. Genetic testing for prevention of severe drug-induced skin rash. Cochrane Database Syst Rev. 2019;7: CD010891
VI. Han XD, Koh MJA, Wong SMY. Drug reaction with eosinophilia and systemic symptoms in a cohort of Asian children. Pediatr Dermatol. 2019;36:324-329.
VII. Mizukawa Y, Hirahara K, Kano Y, Shiohara T. Drug-induced hypersensitivity syndrome/drug reaction with eosinophilia and systemic symptoms severity score: A useful tool for assessing disease severity and predicting fatal cytomegalovirus disease. J Am Acad Dermatol. 2019;80:670-678.
VIII. Kim D, Kobayashi T, Voisin B, Jo JH, et ál. Targeted therapy guided by single-cell transcriptomic analysis in drug-induced hypersensitivity syndrome: a case report. Nat Med. 2020;26:236-243.
IX. Walsh S, Diaz-Cano S, Higgins E, Morris-Jones R, et ál. Drug reaction with eosinophilia and systemic symptoms: is cutaneous phenotype a prognostic marker for outcome? A review of clinicopathological features of 27 cases. Br J Dermatol. 2013;168:391-401.
X. Husain Z, Reddy BY, Schwartz RA. DRESS syndrome: Part I. Clinical perspectives. J Am Acad Dermatol. 2013;68:693.e1-14.
XI. Lee JY, Lee SY, Hahm JE, Ha JW, et ál. Clinical features of drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome: a study of 25 patients in Korea. Int J Dermatol. 2017;56:944-951.
XII. Aihara M. Pharmacogenetics of cutaneous adverse drug reactions. J Dermatol. 2011;38:246-254.
XIII. Chen CB, Wu MY, Ng CY, Lu C-W, et ál. Severe cutaneous adverse reactions induced by targeted anticancer therapies and immunotherapies. Cancer Manag Res. 2018;10:1259-1273.
XIV. Duong TA, Valeyrie-Allanore L, Wolkenstein P, Chosidow O. Severe cutaneous adverse reactions to drugs. Lancet. 2017;390:1996-2011.
XV. Naranjo CA, Busto U, Sellers EM, Sandor P, et ál. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981;30:239-245.
XVI. Descamps V, Ranger-Rogez S. DRESS syndrome. Joint Bone Spine. 2014;81:15-21.
XVII. Shiohara T, Mizukawa Y. Comment on “Drug reaction with eosinophilia and systemic symptoms syndrome in a patient with COVID‐19”: involvement of herpesvirus reactivations and adverse drug reactions in diverse cutaneous manifestations and overall disease severity of COVID‐19. J Eur Acad Dermatol Venereol. 2021;35:98-100.
XVIII. Mallal S, Nolan D, Witt C, Masel G, et ál. Association between presence of HLA-B*5701, HLA-DR7, and HLA-DQ3 and hypersensitivity to HIV-1 reverse-transcriptase inhibitor abacavir. Lancet. 2002;359:727–732.
XIX. Illing PT, Purcell AW, McCluskey J. The role of HLA genes in pharmacogenomics: unravelling HLA associated adverse drug reactions. Immunogenetics. 2017;69:617-630.
XX. Criado PR, Criado RFJ, de Magalhães Avancini J, Santi CG. Drug reaction with Eosinophilia and Systemic Symptoms (DRESS)/Drug-induced Hypersensitivity Syndrome (DIHS): a review of current concepts. An Bras Dermatol. 2012;87:435-449.
XXI. Anil H, Harmanci K, Tekin RT, Kocak A. Presence of a single nucleotide polymorphism (RS3758581) in a boy with DRESS syndrome. Cent Eur J Immunol. 2017;42:409-411.
XXII. Redwood AJ, Pavlos RK, White KD, Phillips EJ. HLAs: Key regulators of T-cell-mediated drug hypersensitivity. HLA. 2018;91:3-16.
XXIII. Bellón T. Mechanisms of severe cutaneous adverse reactions: recent advances. Drug Saf. 2019;42:973-992.
XXIV. Illing PT, Mifsud NA, Purcell AW. Allotype specific interactions of drugs and HLA molecules in hypersensitivity reactions. Curr Opin Immunol. 2016;42:31-40.
XXV. Sugita K, Tohyama M, Watanabe H, Otsuka A, et ál. Fluctuation of blood and skin plasmacytoid dendritic cells in drug-induced hypersensitivity syndrome. J Allergy Clin Immunol. 2010;126:408-410.
XXVI. Shiohara T, Kano Y. A complex interaction between drug allergy and viral infection. Clin Rev Allergy Immunol. 2007;33:124-133.
XXVII. Hirahara K, Kano Y, Mitsuyama Y, Takahashi R, et ál. Differences in immunological alterations and underlying viral infections in two well-defined severe drug eruptions. Clin Exp Dermatol. 2010;35:863-868.
XXVIII. Martínez-Cabriales SA, Rodríguez-Bolaños F, Shear NH. Drug reaction with eosinophilia and systemic symptoms (DReSS): How far have we come? Am J Clin Dermatol. 2019;20:217-236.
XXIX. Riganti J. El rol de las infecciones por herpesvirus-6, herpesvirus-7, virus Epstein-Barr y citomegalovirus en las farmacodermias. Dermatol Argent. 2014;20:17-26.
XXX. Cura MJ, Torre AC, Cueto Sarmiento KY, Bollea Garlatti ML, et ál. Reticular rash in drug reaction with eosinophilia and systemic symptoms syndrome: A clue to parvovirus B19 reactivation? JAAD Case Rep. 2018;4:728-732.
XXXI. Raschi E, Antonazzo IC, La Placa M, Ardizzoni A, et ál. Serious cutaneous toxicities with immune checkpoint inhibitors in the U.S. Food and Drug Administration Adverse Event Reporting System. Oncologist. 2019;24:1128-1131.
XXXII. Kardaun SH, Sidoroff A, Valeyrie-Allanore L, Halevy S, et ál. Variability in the clinical pattern of cutaneous side-effects of drugs with systemic symptoms: does a DRESS syndrome really exist? Br J Dermatol. 2007;156:609-611.
XXXIII. Jeung YJ, Lee JY, Oh MJ, Choi DC, et ál. Comparison of the causes and clinical features of drug rash with eosinophilia and systemic symptoms and Stevens-Johnson syndrome. Allergy Asthma Immunol Res. 2010;2:123-126.
XXXIV. Ganeva M, Gancheva T, Lazarova R, Troeva J, et ál. Carbamazepine-induced drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome: report of four cases and brief review. In J Dermatol. 2008;47:853-860.
XXXV. De A, Rajagopalan M, Sarda A, Das S, et ál. Drug Reaction with eosinophilia and systemic symptoms: an update and review of recent literature. Indian J Dermatol. 2018;63:30-40.
XXXVI. Lin IC, Yang HC, Strong C, Yang CW, et ál. Liver injury in patients with DRESS: A clinical study of 72 cases. J Am Acad Dermatol. 2015;72:984-991.
XXXVII. Ghabril M, Chalasani N, Björnsson E. Drug-induced liver injury: a clinical update. Curr Opin Gastroenterol. 2010;26:222-226.
XXXVIII. Ichai P, Laurent-Bellue A, Saliba F, Moreau D, et ál. Acute liver failure/injury related to drug reaction with eosinophilia and systemic symptoms: outcomes and prognostic factors. Transplantation. 2017;101:1830-1837.
XXXIX. Chen YC, Chiu HC, Chu CY. Drug reaction with eosinophilia and systemic symptoms: a retrospective study of 60 cases. Arch Dermatol. 2010;146:1373-1379.
XL. Kano Y, Ishida T, Hirahara K, Shiohara T. Visceral involvements and long-term sequelae in drug-induced hypersensitivity syndrome. Med Clin North Am. 2010; 94:743–759.
XLI. Shiohara T, Iijima M, Ikezawa Z, Hashimoto K. The diagnosis of a DRESS syndrome has been sufficiently established on the basis of typical clinical features and viral reactivations. Br J Dermatol. 2007;156:1083-1084.
XLII. Ushigome Y, Kano Y, Hirahara K, Shiohara T. Human herpesvirus 6 reactivation in drug-induced hypersensitivity síndrome and DRESS validation score. Am J Med. 2012;125:9-10.
XLIII. Ortonne N, Valeyrie Allanore L, Bastuji Garin S, Wechsler J, et ál. Histopathology of drug rash with eosinophilia and systemic symptoms syndrome: a morphological and phenotypical study. Br J Dermatol. 2015;173:50-58.
XLIV. Chi MH, Hui RC, Yang CH, Lin JY, et ál. Histopathological analysis and clinical correlation of drug reaction with eosinophilia and systemic symptoms (DRESS). Br J Dermatol. 2014;170:866-873.
XLV. Torre AC, Hidalgo-Parra I, La Forgia MP, Noguera M, et ál. Guías de evaluación, diagnóstico y tratamiento de las reacciones adversas cutáneo mucosas graves más frecuentes. Sociedad Argentina de Dermatología - SAD. 2020; 1. Disponible en: https://sad.org.ar/wp-content/uploads/2020/06/Guiade-evaluaci%C3%B3n-diagn%C3%B3stico-y-tratamientoFinal-Abril.pdf . [Consultado noviembre 2021].
XLVI. Husain Z, Reddy BY, Schwartz RA. DRESS syndrome: Part II. Management and therapeutics. J Am Acad Dermatol. 2013;68:718-720.
XLVII. Funck-Brentano E, Duong TA, Bouvresse S, Bagot M, et ál. Therapeutic management of DRESS: a retrospective study of 38 cases. J Am Acad Dermatol. 2015;72:246-252.
XLVIII. Bayan CAY, Lopez A, Fontecilla NM, Geskin LJ. Successful treatment of drug reaction with eosinophilia and systemic symptoms syndrome relapse with oral pulsed dexamethasone. JAAD Case Rep. 2018;4:959-961.
XLIX. Natkunarajah J, Goolamali S, Craythorne E, Benton E, et ál. Ten cases of drug reaction with eosinophilia and systemic symptoms (DRESS) treated with pulsed intravenous methylprednisolone. Eur J Dermatol. 2011;21:385-391.
L. Descamps V, Ben Saïd B, Sassolas B, Truchetet F, et ál. Management of drug reaction with eosinophilia and systemic symptoms (DRESS). Ann Dermatol Venereol. 2010;137:703-70
LI. Ingen-Housz-Oro S, Duong TA, de-Prost N, Colin A, et ál. Treatment of severe cutaneous adverse drug reactions. Ann Dermatol Venereol. 2018; 145:454-464.
LII. Joly P, Janela B, Tetart F, Rogez S, et ál. Poor benefit/risk balance of intravenous immunoglobulins in DRESS. Arch Dermatology. 2012;148:543-544.
LIII. Mushiroda T, Takahashi Y, Onuma T, Yamamoto Y, et ál. Association of HLA-A* 31: 01 screening with the incidence of carbamazepine-induced cutaneous adverse reactions in a Japanese population. JAMA Neurol. 2018;75:842-849.
LIV. Oussalah A, Yip V, Mayorga C, Blanca M, et ál. Genetic variants associated with T cell–mediated cutaneous adverse drug reactions: A PRISMA‐compliant systematic review- An EAACI position paper. Allergy. 2020;75:1069-1098.
LV. Chang CJ, Chen CB, Hung SI, Ji C, et ál. Pharmacogenetic testing for prevention of severe cutaneous adverse drug reactions. Front Pharmacol. 2020;11:969-980.
LVI. Konvinse KC, Trubiano JA, Pavlos R, James I, et ál. HLA-A*32:01 is strongly associated with vancomycin-induced drug reaction with eosinophilia and systemic symptoms. J Allergy Clin Immunol. 2019;144:183-192.
Downloads
Published
Issue
Section
License
Copyright (c) 2022 Dermatología Argentina

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
El/los autor/es tranfieren todos los derechos de autor del manuscrito arriba mencionado a Dermatología Argentina en el caso de que el trabajo sea publicado. El/los autor/es declaran que el artículo es original, que no infringe ningún derecho de propiedad intelectual u otros derechos de terceros, que no se encuentra bajo consideración de otra revista y que no ha sido previamente publicado.
Le solicitamos haga click aquí para imprimir, firmar y enviar por correo postal la transferencia de los derechos de autor